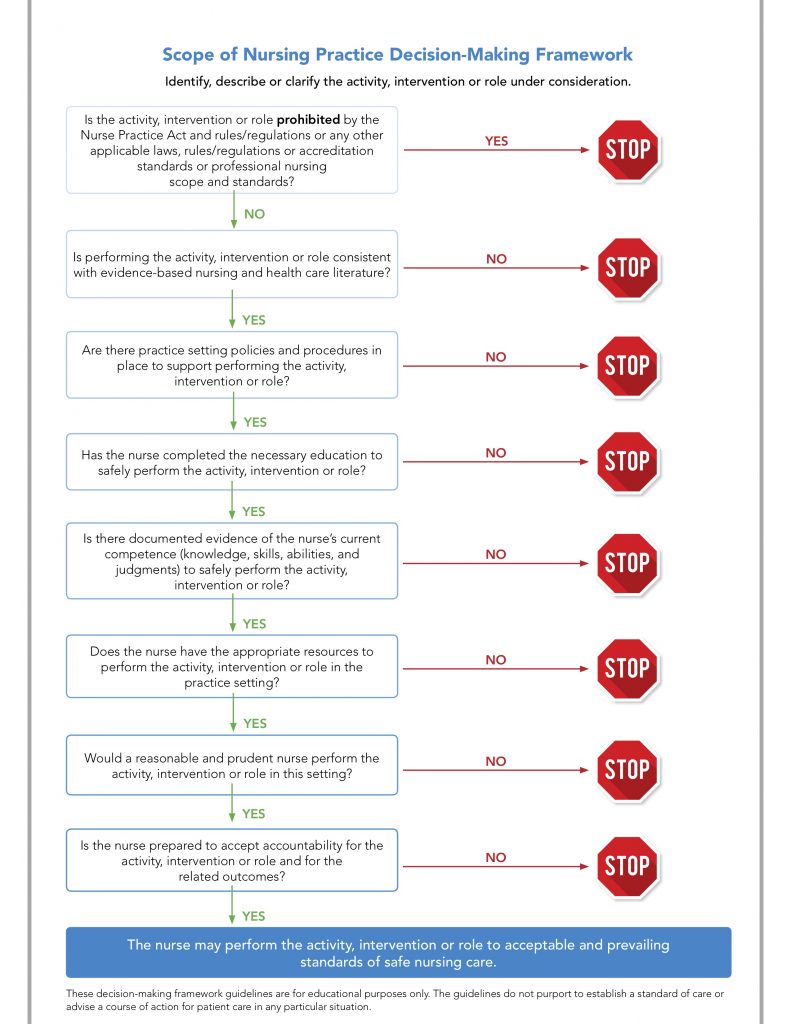
To assist nurses, employers and patients, the National Council of State Boards of Nursing (NCSBN) has developed a Scope of Practice Decision-Making Framework to be used when determining whether a particular nursing activity is within the nurse’s scope of practice. It is very straightforward. Most states have implemented/recommended this decision-making algorithm, and I encourage all nurses to use it in their practice. This framework includes a series of questions that should be asked before performing a nursing act about which you are uncertain. This month, our Nursing Behind the Wall case study will allow us to practice using this framework.
Joan Miller, Registered Nurse
Today, RN Miller is the nurse covering Nurse Sick Call (NSC) at the county jail. She has been a nurse for 15 years, and the last five have been at the jail. She has been oriented to the Nursing Protocols used in NSC, although this is not a regular assignment for her. Mr. Greene arrives to NSC with a complaint of a “spider bite” in his left axilla that he noticed about three days ago. At that time, he was seen in NSC by another registered nurse, who contacted the provider and received an order for Bactrim DS – one tablet twice a day for 10 days. Today Mr. Greene complains that the pain is “excruciating” and it needs to be opened. He informs RN Miller that he “gets them all the time” and so he is sure that opening the abscess and letting it drain will bring huge relief. He tells her that all she had to do is use “the knife” and just knick the skin. Ms. Miller assesses the lesion and finds that it has doubled in size from the initial description documented two days ago in Mr. Greene’s health record. It is moveable and ‘squishy”, and extremely tender to light palpation. RN Miller’s past experience was in med-surg, but she has been helping the providers there at the jail and has witnessed many wound incision and drainage procedures (I&D). There are no providers scheduled onsite for the next two days. Although she is not sure that she should be opening the abscess, she ultimately decides that this is what is best for her patient, and so RN Miller gets the scalpel with the #15 blade and uses clean technique to make a small puncture in the lesion, which immediately starts draining light, coffee colored pus. Once the drainage stops, RN Miller dresses the lesion, and makes sure that Mr. Greene is scheduled for nursing wound care, which he is. Mr. Greene is very grateful, and immediately reports that the pain is already easing. In the next two weeks, Mr. Greene is adherent to his antibiotic and wound care regimen, and the wound heals with no complications.
A colleague at the jail was so concerned about RN Miller’s actions that he contacted the Board of Nursing and a formal investigation was initiated. As a result of the inquiry from the Board of Nursing, the supervisor and medical director at the jail wrote a formal reprimand that is now included in her personnel folder.
If RN Miller had stopped and considered the action (conducting an I&D on Mr. Greene’s abscess) using the Scope of Practice Decision-Making Framework, she would not be under investigation with the Board of Nursing, nor would she have a formal reprimand in her personnel file.
The Framework
Is the activity, intervention or role prohibited by the Nurse Practice Act and rules/regulations or any other applicable laws, rules/regulations or accreditation standards or professional nursing scope and standards?
No, although at the time of her decision, RN Miller did not know the Nurse Practice Act in her state.
Is performing the activity, intervention or role consistent with evidence-based nursing and healthcare literature?
Yes, there is evidence to support opening an abscess so that more efficient drainage will occur.
Are there practice setting policies and procedures in place to support performing the activity, intervention or role?
No, there is no policy or procedure at the jail that supports RNs doing I&Ds…so this would be a STOP and RN Miller should not continue with her plan to open the abscess.
While this is the point where RN Miller should have STOPPED, let’s go on to a few more questions from the framework to show that, even if she missed the first STOP, the next two questions would have definitely caused her to put down the scalpel!
Has the nurse completed the necessary education to safely perform the actively, intervention or role?
NO – RN Miller has never had training in incision and drainage and this would be another STOP.
Is there evidence of the nurse’s current competence (knowledge, skills, abilities, and judgments) to safely perform the activity, intervention or role?
NO – RN Miller had no evidence of current competency performing abscess incision and drainage in her personnel folder. This would be another STOP.
Summary
If RN Miller had taken a few moments and reviewed the actions she wanted to take with reference to the NCSBN’s Scope of Nursing Practice Decision-Making Framework, then she would have known that performing an incision and drainage (opening the abscess) was outside of her scope of practice as a registered nurse in that state and in that facility, and she should not have done it. She would have realized this at the third step, when she determined that there was no policy or procedure that supported an RN performing an I&D. Her next step would have been to contact a provider to determine what to do for Mr. Greene.
Do you consider your scope of practice through reviewing the Nurse Practice Act and the policies and procedures at your facility to determine if a particular activity is within your scope of practice? Please share your experiences with this very important part of your nursing practice in the comments section below.
Robin Noel Bennett says
For many of us these steps are done almost subconsciously. But as I have progressed there have for sure been moments I have had to mentally step back and review tasks es in a new setting or role.
Great reminder for everyone.
I love that the steps also remind us to be aware of what we have been trained to do. Just because the law says we can doesnt always mean we should.