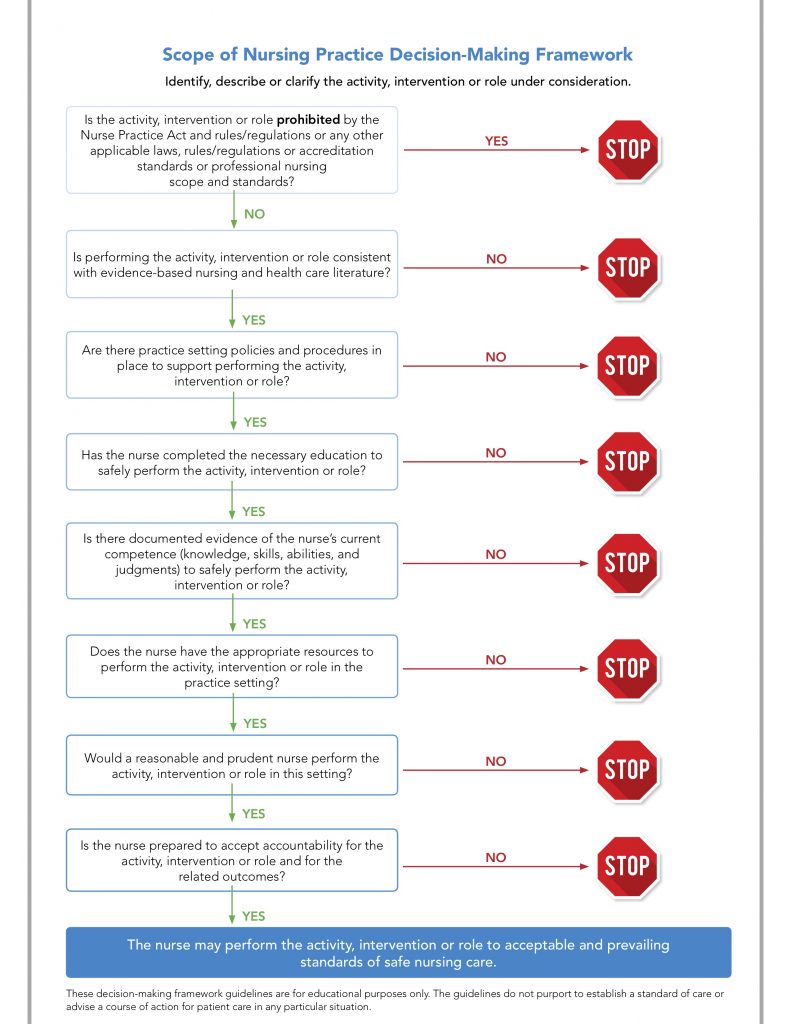
To assist nurses, employers and patients, the National Council of State Boards of Nursing (NCSBN) has developed a Scope of Practice Decision-Making Framework to be used when determining whether a particular nursing activity is within the nurse’s scope of practice. It is very straightforward. Most states have implemented/recommended this decision-making algorithm, and I encourage all nurses to use it in their practice. This framework includes a series of questions that should be asked before performing a nursing act about which you are uncertain. This is our second monthly Nursing Behind the Wall case study that will allow us to practice using this framework.
Caitlin Roberts, Licensed Practical Nurse
Caitlin Roberts is an LPN who has been practicing for 20 years, with the last 15 years in correctional healthcare. She works in a small county jail with an average daily census of 175 detainees. She is the nurse in charge, and there are 3 other nurses and 2 PRN staff with whom she works. There is a physician on-call 24/7 who also comes onsite weekly to see patients. LPN Roberts has always instructed the officers to call her with any questions or patient problems, and she will contact the physician, if she thinks that needs to be done. She is very proud of the work she does as a correctional nurse, and believes that she is really helping her patients and community.
One Saturday evening she received a call from Officer Barister informing her that there was a new diabetic patient just admitted who told him that he took 70/30 insulin, 20 units in the morning and 10 units in the evening. In addition, the patient (Mr. Murphy) also told Officer Barister that he uses regular insulin as “coverage.” LPN Roberts tells Officer Barister that she will keep Mr. Murphy on these dosages, and to place Mr. Murphy on the twice daily blood glucose list. Mr. Murphy’s wife brings in his insulin the next morning.
On the second night, LPN Roberts received a call from Officer Jones stating that Mr. Murphy felt like his blood sugar was elevated and he felt shaky and sweaty, so Officer Jones checked it and it was 288. LPN Roberts instructed Officer Jones to use the sliding scale. She also told Officer Jones that a 288 blood sugar didn’t really concern her, because she has seen plenty of individuals with diabetes whose blood sugar was routinely higher than that.
That next morning, Mr. Murphy’s blood glucose was 240, and he self-administered his basal insulin (20 units of 70/30). He saw LPN Roberts when she arrived at the jail, and told her that his blood glucose normally ran in the 130’s at home. LPN Roberts told him not to worry, that most often the diet at the jail is not really conducive to maintaining glucose control for diabetics, and that he was really doing fine, “considering.”
The third night, LPN Roberts received a telephone call from Officer Barister that Mr. Murphy was acting confused, and was tremulous and sweaty. LPN Roberts instructed Officer Barrister to ask Mr. Murphy if he had taken any drugs from another inmate, or if he was detoxing from any street drugs that he “forgot” to tell them about at intake. Mr. Murphy could not really understand the questions asked, and did not respond appropriately. LPN Roberts instructed Officer Barrister to place Mr. Murphy in medical observation and she would see him in the morning.
Three hours later, Mr. Murphy was found unresponsive on the floor of his medical observation cell. Emergency Medical Services was activated, and when they arrive, they tested Mr. Murphy’s blood glucose, which was 520. Mr. Murphy received the treatment his ketoacidosis required from the local emergency department. He was released from the jail while he was in the hospital, and so he never returned to the facility.
Two months later, LPN Roberts received a certified letter from the state Board of Nursing informing her that she was under investigation for significantly exceeding her scope of practice as an LPN in the care she provided to Mr. Murphy. Her questionable actions cited included ordering medication, determining a chronic disease patient’s treatment plan, and not consulting with a provider for a patient with an abnormal medical finding. LPN Roberts was very upset because she treated Mr. Murphy the same as she has treated every other patient she cared for at the facility for the last 15 years, which was with compassion and using her “nursing clinical judgment.”
Did LPN Roberts practice beyond her scope?
The Framework
Is the activity, intervention or role prohibited by the Nurse Practice Act and rules/regulations or any other applicable laws, rules/regulations or accreditation standards or professional nursing scope and standards?
Yes – the ordering of medication is prohibited by the Nurse Practice Act. But, LPN Roberts believes that she did not “order” medication; she was merely following the orders/prescription of Mr. Murphy’s personal provider. When questioned as part of the investigation, Mr. Murphy’s personal provider stated that he had nothing to do with the jail or its healthcare program, and he was not LPN Roberts’ supervisor. He did not give her the order to continue the medication.
If LPN Roberts had contacted the provider from the jail to get an order for Mr. Murphy’s insulin, “ordering medication” would not be on the citation list.
In LPN Roberts’ state, LPNs can add to the assessment of a patient by collecting data, which then must be reported to someone with the licensure that allowed determination of a plan of care/treatment for the patient. LPN Roberts made patient treatment determinations about abnormal findings without calling the provider, which is prohibited by her state Nurse Practice Act.
LPN Roberts should have STOPPED here if she was following the NCSBN Scope of Nursing Practice Decision-Making Framework, but let’s go on to see how the other criteria fit in.
Is performing the activity, intervention or role consistent with evidence-based nursing and healthcare literature?
Monitoring blood glucose is consistent with evidence-based nursing literature. LPNs ordering medication is not consistent with evidence-based nursing literature, nor is LPNs making treatment decisions for a patient with an abnormal finding without consulting a provider.
Even if she missed the first criteria that indicated she should STOP, LPN Roberts should have STOPPED here if she was following the NCSBN Scope of Nursing Practice Decision-Making Framework, but let’s go to one more criteria.
Are there practice setting polices and procedures in place to support performing the activity, intervention or role?
Interestingly, the policies and procedures at this jail do allow the nursing staff to “reorder” medication from the patient’s community provider, if they can get verification of the medication and its dosage. In this case, LPN Roberts never verified her patient’s medication; she took the officer’s word about the dosages relayed to him, and so she did not follow her policies and procedures.
The policies and procedures instruct the nurses to call the on-call provider “when needed.” They do not allow independent decision making by the LPN about abnormal findings.
While LPN Roberts should have STOPPED back in the first step of the Framework, even if she missed the first STOP, the next two “No” answers would have definitely caused her to STOP practicing beyond her scope.
Summary
If LPN Roberts had taken a few moments and reviewed the actions she wanted to take with reference to the NCSBN’s Scope of Nursing Practice Decision-Making Framework, then she would have known that ordering medication and determining “next steps” for a diabetic patient with abnormal findings without contacting the on-call provider was outside of her scope of practice as a licensed practical nurse in that state and she should not have done it. She would have realized this at the first step, when she determined that the LPN performing independent assessment and planning was prohibited by her state Nurse Practice Act to do so. Her next step should have been to contact a provider to determine what to do for Mr. Murphy.
Do you consider your scope of practice through reviewing the Nurse Practice Act and the policies and procedures at your facility to determine if a particular activity is within your scope of practice? Do you ensure that you are trained and demonstrate proficiency in any task that you are assigned to perform? Please share your experiences with this very important part of your nursing practice in the comments section below.
Leave a Reply